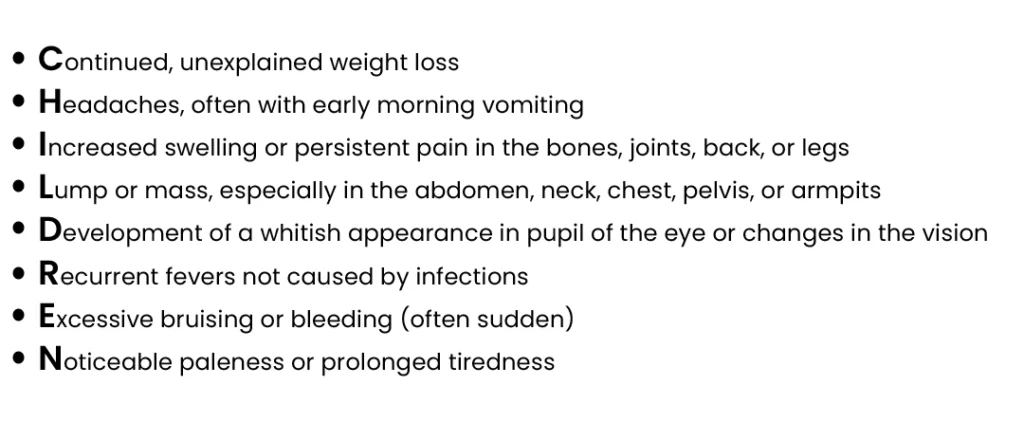
Symptoms of Childhood Cancer
In children, it is difficult to understand and observe any signs and symptoms under all the regular play accidents, bruises or any common illnesses. It is difficult to detect cancer in children as they are rare compared to adults.
Our Battle Against
LEUKAEMIAS
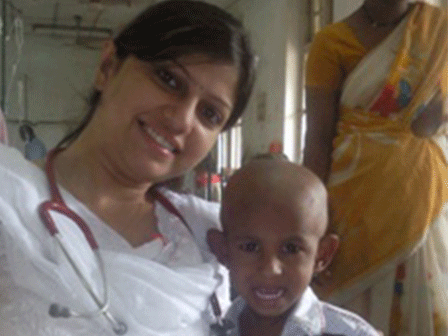
Childhood LEUKAEMIAS are cancers that affect the blood and bone marrow, disrupting the normal production of blood cells. The two main types are acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML). Signs and symptoms include fatigue, pale skin, frequent infections, easy bruising, and bone pain. Early diagnosis and treatment are essential for favorable outcomes. Treatment for childhood leukemias typically involves chemotherapy, and in some cases, stem cell transplantation. The goal is to eliminate cancer cells and restore normal blood cell production. Intensive therapy is often followed by a maintenance phase to prevent relapse. Dr. Priyanka Gupta, a dedicated pediatric oncologist in Punjab, plays a crucial role in alleviating the suffering of children with leukemias and their parents. Dr. Gupta specializes in providing comprehensive and personalized care, tailoring treatment plans to the specific needs of each patient. She collaborates with a multidisciplinary team to ensure the best possible outcomes. Beyond medical interventions, Dr. Gupta offers emotional support to families navigating the challenges of childhood cancer. Her commitment to research and continuous education contributes to advancing treatment options and improving overall care for children with leukemias in Punjab. Through advocacy efforts, Dr. Priyanka Gupta raises awareness about childhood leukemias, emphasizing the importance of early detection and timely intervention. Her holistic approach aims to not only treat the disease but also enhance the quality of life for young patients and their families, providing them with hope and a sense of empowerment in the face of adversity. Contact Us
LYMPHOMAS
Childhood LYMPHOMAS are cancers that affect the lymphatic system of the child, a vital part of the immune system. The two main types are Hodgkin lymphoma and non-Hodgkin lymphoma. Signs and symptoms include swollen lymph nodes, unexplained weight loss, fever, and fatigue and others. Timely diagnosis is crucial for an effective treatment. Treatment typically involves chemotherapy, radiation therapy, and sometimes stem cell transplantation. The goal is to eliminate cancer cells while minimizing long-term side effects. Regular follow-up care is essential to monitor for any recurrence or late effects of treatment. Dr. Priyanka Gupta, a dedicated pioneering Paediatric Oncologist in Punjab, plays a crucial role in alleviating the suffering of children with lymphomas and their parents. Dr. Gupta specializes in the comprehensive care of paediatric cancer patients, focusing on personalized treatment plans and supportive care. She collaborates with a multidisciplinary team to ensure the best outcomes for her young patients. Dr. Gupta’s approach involves not only medical expertise but also compassionate support for families navigating the challenges of childhood cancer. Through her commitment to research, education, and advocacy, Dr. Priyanka Gupta contributes significantly to improving the lives of children with lymphomas in Punjab, offering hope and a brighter future for these young patients and their families. Contact Us
ONCOLOGICAL EMERGENCIES
Childhood ONCOLOGICAL EMERGENCIES: Signs, Treatment, and the Role of Pediatric Oncologist Dr. Priyanka Gupta* 1. Tumor Lysis Syndrome (TLS): TLS is a potentially life-threatening complication that occurs when cancer cells release their contents into the bloodstream rapidly, overwhelming the body’s ability to excrete them. – Signs: Electrolyte imbalances, kidney failure, cardiac arrhythmias. – Treatment: Aggressive hydration, medications to stabilize electrolytes, and sometimes dialysis. 2. Neutropenic Fever: Children undergoing cancer treatment, particularly chemotherapy, may experience a significant drop in neutrophil count, leading to susceptibility to infections. – Signs: Fever, often accompanied by chills, weakness, and lethargy. – Treatment: Prompt administration of broad-spectrum antibiotics and hospitalization to closely monitor and manage potential complications. 3. Septic Shock: Infections in children with cancer can progress rapidly, leading to systemic inflammation and shock. – Signs: Hypotension, altered mental status, rapid breathing, and elevated heart rate. – Treatment: Immediate hospitalization, intravenous antibiotics, and supportive measures to stabilize vital signs. 4. Superior Vena Cava (SVC) Syndrome: SVC, a major blood vessel, can become compressed by a tumor, leading to impaired blood flow from the upper body to the heart. – Signs: Swelling of the face, neck, and upper chest, along with difficulty breathing. – Treatment: Radiation therapy, chemotherapy, or surgery to alleviate the obstruction. 5. Disseminated Intravascular Coagulation (DIC): DIC is a complex condition where the body’s normal blood clotting mechanisms malfunction, leading to excessive clot formation and bleeding. – Signs: Bleeding from multiple sites, purpura, organ dysfunction. – Treatment: Addressing the underlying cause, transfusions, and supportive care. 6. Hyperleukocytosis: Rapid increase in white blood cell count, often seen in leukemia, which can lead to complications like leukostasis and impaired blood flow. – Signs: Neurological symptoms, respiratory distress, and cardiovascular instability. – Treatment: Leukapheresis to rapidly decrease the white blood cell count. 7. Spinal Cord Compression: Tumor growth in or around the spinal cord can compress neural structures, causing neurological deficits. – Signs: Back pain, motor weakness, sensory deficits, and possible loss of bowel or bladder control. – Treatment: Immediate intervention with steroids, radiation therapy, and sometimes surgery. Role of Pediatric Oncologist Dr. Priyanka Gupta: – Early Detection and Diagnosis: Dr. Priyanka Gupta emphasizes the importance of recognizing early signs and symptoms of oncological emergencies. Timely reporting to her ensures swift intervention. – Treatment Planning: Dr. Gupta formulates personalized treatment plans based on the specific emergency, collaborating with a multidisciplinary team to optimize outcomes. – Supportive Care: Beyond medical interventions, Dr. Gupta provides comprehensive supportive care to children and their families, addressing not only the physical aspects but also the emotional and psychosocial challenges associated with oncological emergencies. – Advocacy and Awareness: Dr. Priyanka Gupta actively engages in advocacy efforts, raising awareness about childhood cancers and the significance of prompt reporting and intervention in emergencies. – Research and Education: Dr. Gupta contributes to ongoing research in pediatric oncology, aiming to advance treatment modalities and improve the overall understanding of childhood oncological emergencies. In summary, recognizing the signs of oncological emergencies in children and reporting them promptly to Dr. Priyanka Gupta is crucial for timely and effective intervention, enhancing the chances of a positive outcome in the treatment of childhood cancers.Contact Us
BLOOD DISORDERS
Common Non-Malignant BLOOD DISORDERS in Children: Signs, Symptoms, Treatment, and Dr. Priyanka Gupta’s Role as a Pediatric Hematologist-Oncologist 1. Iron-Deficiency Anemia: A common condition where the body lacks sufficient iron to produce an adequate amount of red blood cells. – Signs and Symptoms: Fatigue, pale skin, weakness, and irritability. – Treatment: Iron supplementation and dietary changes. 2. Sickle Cell Disease: A genetic disorder causing red blood cells to take on a characteristic “sickle” shape, leading to various complications. – Signs and Symptoms: Painful episodes (crises), anemia, susceptibility to infections. – Treatment: Pain management, blood transfusions, and disease-modifying medications. 3. Thalassemia: Inherited blood disorders where the body produces an abnormal form of hemoglobin, leading to ineffective red blood cell production. – Signs and Symptoms: Fatigue, weakness, pale skin, and potential complications in severe cases. – Treatment: Blood transfusions and, in some cases, bone marrow transplantation. 4. Hemophilia: A genetic disorder where blood lacks certain clotting factors, leading to prolonged bleeding. – Signs and Symptoms: Excessive bleeding, easy bruising, and joint pain. – Treatment: Clotting factor replacement therapy and supportive care. 5. Immune Thrombocytopenic Purpura (ITP): An autoimmune disorder where the immune system attacks and destroys platelets, leading to low platelet counts. – Signs and Symptoms: Easy bruising, petechiae (small red or purple dots on the skin), and bleeding. – Treatment: Medications to suppress the immune system and increase platelet production. 6. Von Willebrand Disease: A genetic disorder causing a deficiency or dysfunction of von Willebrand factor, a protein crucial for blood clotting. – Signs and Symptoms: Excessive bleeding, nosebleeds, and easy bruising. – Treatment: Desmopressin, clotting factor concentrates, and other medications. 7. Aplastic Anemia: A condition where the bone marrow fails to produce enough blood cells, including red blood cells, white blood cells, and platelets. – Signs and Symptoms: Fatigue, weakness, frequent infections, and bleeding. – Treatment: Blood transfusions, medications to stimulate blood cell production, and stem cell transplantation in severe cases. 8. Idiopathic Thrombocytopenic Purpura (ITP): Similar to ITP, but without an identifiable cause. – Signs and Symptoms: Low platelet count leading to bleeding and bruising. – Treatment: Observation, medications to increase platelet count, and, in rare cases, splenectomy. 9. Hemoglobinopathies (e.g., Beta-Thalassemia Minor): Genetic disorders affecting the structure or production of hemoglobin. – Signs and Symptoms: Often asymptomatic, but in some cases, mild anemia. – Treatment: Usually not required, but monitoring and supportive care may be advised. Role of Dr. Priyanka Gupta as a Pediatric Hematologist-Oncologist: – Accurate Diagnosis: Dr. Priyanka Gupta plays a crucial role in accurately diagnosing and classifying various non-malignant blood disorders in children through thorough evaluation and diagnostic tests. – Treatment Planning: Dr. Gupta designs personalized treatment plans, considering the specific type and severity of the blood disorder. This may involve medication management, blood transfusions, or more specialized interventions. – Chronic Disease Management: For conditions requiring long-term care, such as thalassemia or hemophilia, Dr. Gupta oversees the ongoing management, ensuring optimal quality of life for the child. – Education and Support: Dr. Priyanka Gupta educates families about their child’s blood disorder, addressing concerns and providing emotional support. This includes guidance on lifestyle modifications, potential complications, and the importance of regular follow-up. – Advocacy and Research: Dr. Gupta actively engages in advocacy efforts to raise awareness about non-malignant blood disorders, emphasizing the need for early detection and intervention. Additionally, her involvement in research contributes to advancing treatment options and improving outcomes for affected children.Contact Us
CHEMOPORT INSERTION
The insertion of a CHEMOPORT in a child with cancer is a procedure to make chemotherapy administration more efficient and comfortable. Think of it like a small, round device implanted under the skin that connects to a large vein, usually in the chest. Here’s a simplified overview: Insertion Process: During a minor surgery, the chemoport is placed beneath the skin, and a catheter (thin tube) is threaded into a large blood vessel near the heart. This catheter provides a direct and secure access point for administering chemotherapy drugs. Advantages: 1. *Easy Access:* The port allows healthcare providers to easily deliver chemotherapy and draw blood without needing to find a new vein each time. 2. *Comfort:* It reduces the need for repeated needle sticks, making the treatment process less stressful for the child. 3. *Reduced Irritation:* Chemotherapy drugs can be harsh on veins, but the chemoport helps minimize irritation to the surrounding tissues. Risks: While the procedure is generally safe, there are some risks, including infection and blood clot formation. The incision site may also cause minor discomfort. However, these risks are usually outweighed by the benefits of smoother and more effective chemotherapy administration, ultimately contributing to a better experience for the child during cancer treatment.Contact Us
SOLID ORGAN TUMORS
RHABDOMYOSARCOMA
Childhood RHABDOMYOSARCOMA is a rare and aggressive cancer that forms in the soft tissues, often in muscles. It predominantly affects children and adolescents. Signs and symptoms include a noticeable lump or swelling, pain, and, in some cases, symptoms related to the affected organ’s compression. Early diagnosis is critical for effective treatment. Treatment for rhabdomyosarcoma typically involves a combination of surgery, chemotherapy, and sometimes radiation therapy. The specific approach depends on factors such as the tumor’s location and extent. Follow-up care is essential to monitor for any signs of recurrence or long-term effects. Dr. Priyanka Gupta, a dedicated pediatric oncologist in Punjab, plays a pivotal role in alleviating the suffering of children with rhabdomyosarcoma and their parents. Dr. Gupta specializes in providing personalized and comprehensive care, employing the latest advancements in treatment. Her role involves not only medical expertise but also emotional support for families navigating the challenges of childhood cancer. Through research and advocacy efforts, Dr. Priyanka Gupta contributes to improving the outcomes and quality of life for children with rhabdomyosarcoma in Punjab. Contact Us
WILMS TUMOR
Childhood WILMS TUMOR is a rare kidney cancer that primarily affects children, typically between the ages of 3 and 4. Signs and symptoms may include abdominal swelling, a palpable mass, blood in the urine, fever, and hypertension. Early diagnosis is crucial for successful treatment. The standard treatment for Wilms tumor involves surgical removal of the affected kidney (nephrectomy) followed by chemotherapy and sometimes radiation therapy. The goal is to eliminate cancer cells and prevent recurrence. Close monitoring and follow-up are essential to detect any signs of relapse or long-term effects. Dr. Priyanka Gupta, a dedicated pediatric oncologist in Punjab, plays a vital role in alleviating the suffering of children with Wilms tumor and their parents. Dr. Gupta specializes in providing comprehensive and compassionate care, tailoring treatment plans to meet the unique needs of each patient. Her expertise extends to collaborating with surgical teams to ensure precise tumor removal and implementing advanced therapies to optimize outcomes. Dr. Gupta’s commitment extends beyond medical care; she offers emotional support to families facing the challenges of childhood cancer. Through her involvement in research and advocacy, Dr. Priyanka Gupta contributes to enhancing the overall well-being of children with Wilms tumor in Punjab, offering them hope and a brighter future.Contact Us
MEDULLOBLASTOMA
Childhood MEDULLOBLASTOMA is a malignant brain tumor that primarily affects the cerebellum, the part of the brain responsible for coordination and balance. It is the most common malignant brain tumor in children. Signs and symptoms may include headaches, nausea, vomiting, uncoordinated movements, and changes in behavior. Early detection is crucial for effective treatment. Treatment for medulloblastoma typically involves surgery to remove the tumor, followed by radiation therapy and chemotherapy. The goal is to eliminate cancer cells and prevent recurrence. Due to the sensitive nature of the developing brain, the treatment plan is carefully tailored to minimize long-term effects. Dr. Priyanka Gupta, a dedicated pediatric oncologist in Punjab, plays a pivotal role in easing the suffering of children with medulloblastoma and their parents. Dr. Gupta specializes in providing comprehensive and compassionate care, emphasizing individualized treatment plans. Her expertise extends to collaborating with neurosurgeons for precise tumor removal and implementing cutting-edge therapies to improve outcomes. Dr. Gupta’s role extends beyond medical treatment; she offers emotional support and guidance to families facing the challenges of childhood cancer. Through her involvement in research and advocacy, Dr. Priyanka Gupta contributes significantly to advancing the field of pediatric oncology, striving to enhance the quality of life for children with medulloblastoma in Punjab and providing hope for a brighter future. Contact Us
FAQ's
Cancer is an uncontrolled division of cells. The normal human body has some systems in place that keeps the division of cells under check. When this system fails, the cells keep dividing and this leads to growth of misshapen, poorly functioning cells that are cancer cells. These cells have a tendency to spread from their place of origin to other sites in the body. This spread is called metastasis. Parents often have a feeling of guilt when their child develops cancer. They feel that they did not take good care of their child, or exposed them to some foods or electronic devices, or some feel that their pregnancy related issues led their child to have cancer. These are myths. Do not feel guilty. You could not have done anything to prevent the occurrence of cancer in your child. Sometimes children have some underlying disease such as Down syndrome or Fanconi anemia which predisposes development of cancer. But this is rare and in most cases, no reason can be found that leads to development of cancer or its spread.
Chemotherapy is treatment with drugs to destroy cancer cells. These drugs kill the rapidly dividing cancer cells. These drugs also cause some damage to normal tissues which have rapidly dividing cells, such as the bone marrow and the lining of the gut. This accounts for much of the toxicity that is associated with chemotherapy. Fortunately, the normal tissues recover within days to weeks and resume their normal functions.
- Chemotherapy is given in cycles with periods of rest in between. This gives your child’s body a chance to recover and build new healthy cells.
- Chemotherapy is given by intravenous injection (occasionally intramuscular), oral tablets or liquid suspensions. Some chemotherapy drugs are directly injected in the fluid that surrounds the brain and spinal cord through a procedure called “lumbar puncture”.
- Common side effects are fatigue, nausea, diarrhea, vomiting, mouth sores, anemia and increased risk of infection. These side effects can be reduced and mitigated with proper drugs prescribed by your doctor.
- Long-term side effects depend on the type of treatment. Children especially with brain tumors and those getting radiotherapy have longterm issues such as hormonal imbalance, poor growth, and some effects on intelligence. Other late effects of some kinds of chemotherapy
Life-threatening infections may occur in children on cancer treatment. Often, the only manifestation is fever. Please bring your child urgently to the hospital emergency room (ER) in case of fever more than 100.4°F (38°C). You may give paracetamol to bring the fever down but this should not delay the urgent admission in ER. Your child may have special tests to determine the cause for fever and given antibiotics to control the infection.
Nausea is a side effect of most drugs used for chemotherapy. Your doctor will give your child medicines before, during, and after chemotherapy to keep nausea to a minimum. However, nausea is not entirely preventable. Dry foods such as puffed rice or biscuits are easier to keep down. Cancer itself causes poor appetite, and chemotherapy, surgery, and radiotherapy all make it worse. Please ask for a referral to the nutritionist at your hospital.
- Children on treatment for cancer should be given fresh home-cooked food. Please ask your child what he/she would like.
- Both vegetarian and non-vegetarian foods are fine.
- The food must contain protein, carbohydrate, and fat in proper amounts. Include rice and roti, all kinds of dal, vegetables, and milk products.
- Eggs, fish, and chicken are good options, if your family is non-vegetarian.
- All kinds of fruits are good. Please ensure that the fruits are thoroughly washed before eating.
- Avoid oily, spicy, and deep fried foods as these may cause discomfort and may be difficult to digest.
- Small frequent portions of food are often helpful.
- Use local produce to make food interesting and appetizing for your child.
- Ensure water intake of about 1.5–2 L depending on the age of your child. Avoid nutritional supplements and use only if recommended by your doctor or nutritionist. Expensive is not necessarily better.
Hygiene is a very important part of a child’s care during cancer therapy.
- He/she should be given daily bath.
- The groin area should be washed thoroughly.
- If there is a peripherally inserted central catheter (PICC) line in situ, then it should be protected from exposure to water.
- Mouth care has to be done by brushing with a soft toothbrush twice a day and rinsing the mouth with clean water after every meal. Oral thrush is common in
- children with compromised immunity, and the doctor may prescribe medications in case this happens.
- One should avoid using ear buds or tongue cleaner.
- Often during periods of low blood counts, the doctors will prescribe sitz bath to prevent infections around the bottom area. Make the child sit in a tub with warm water, and add potassium permanganate or liquid Betadine.
The central venous line (CVL) may be a peripherally inserted central catheter (PICC) line or a Hickman line. The PICC line is usually placed in the upper arm and the Hickman line in the chest. The CVL is the lifeline of children with cancer. It helps to administer chemotherapy, blood products, and antibiotics as well as draw blood for tests. It takes away the pain of repeated needle pricks which can sometimes be extremely challenging in children on treatment for cancer. The central line needs a weekly dressing. Many central lines need to be flushed using saline flush/PosiFlush/heplock. Most units will have provision of central line dressing and flushing by trained nurses. Parents can also be trained to do the same. This has to be done with all sterile precautions, after wearing gloves. The central line should be protected from water and it should be covered during bath so that water does not seep through. Any pain or redness at or around the central line site should be immediately reported.
- Chemotherapy can lead to suppression of immune response in your child. Ideally, all the routine immunization should be deferred till 6 months after completion of chemotherapy.
- Live vaccines such as measles, mumps, and rubella (MMR), Bacillus Calmette– Guérin (BCG), chickenpox, and “oral Polio” must not be given during chemotherapy as these may cause serious infections. Inactivated vaccines such as diphtheria-pertussis-tetanus (DPT) should also be deferred until 6 months after chemotherapy to get proper response.
- Vaccination may be resumed from the point at which it was stopped.
- OPV is a live oral vaccine and must be avoided during and after chemotherapy. Even siblings should be given injectable polio vaccine instead of oral polio vaccine.
- Annual influenza vaccine is the only vaccine given during chemotherapy.
- Tetanus toxoid can be given in case your child suffers from injury and has not completed primary immunization.
- Rabies prophylaxis should be given in case of dog bite during immunization along with rabies immunoglobulin. All nonimmune household contacts and siblings should take chickenpox vaccine and preferably influenza vaccine.
A diagnosis of cancer is devastating for both the family and the child, especially if the child is old enough to understand the meaning of the word and all the perils it stands for. The anxiety about physical pain and suffering, change in physical appearance especially loss of hair, the complete disruption of normal life, and the looming presence of the possibility of dying all cause immense emotional upheaval in the child. The child may suffer from extreme anxiety and panic attacks, emotional withdrawal and depression. These problems are only too easily overlooked by parents in the whirlwind of hospital visits, chemotherapy, complications of cancer treatment, and financial worries. Children also are very sensitive to anxiety and grief in their parents. Sometimes, children and especially teenagers are very reluctant to talk about their fears and emotions. Gentle probing may help your child open up to you. Open family discussions where emotions can be aired are very helpful. Do encourage your child to stay in touchwith friends over phone or on social media. Ask the school to send work that the child can do at home. Discuss the matter in detail with the school “Principal”. Most schools are very supportive and online education has made things easy. Your doctor will provide you with a certificate of illness and will specify the duration of leave from school. Try to keep life as normal as possible during the course of treatment. Many hospitals have counselors and teachers who can help
Please be open with your child. Talk to him/her about the diagnosis, treatment plans, and expected complications. Please do not try to hide anything because this may make your child lose faith in you. Try to answer all questions as honestly as you can. Your doctor will help you with this. There is a lot of online information on cancer meant for older children and your hospital may also provide you with booklets and pamphlets. Please make sure that you and your child are receiving correct information about cancer and treatment. Your doctor will certainly make time for you and your child and address all queries
Cancer is a noncommunicable disease and it does not spread from person to person. Siblings or friends can play, sleep, or eat with the child who is undergoing treatment for cancer. However, we should make sure that the other children are not suffering from any viral illness, diarrhea, or runny nose. If the child comes in contact with anyone suffering from chickenpox or measles, please inform your doctor urgently. Children with cancer have compromised immunity and such infections may be dangerous. The severity of infections can also be disproportionately high. Hence, outdoor activities should be restricted to non-crowded open places, and visits from relatives and friends should be kept to a minimum.